What is osteochondrosis?
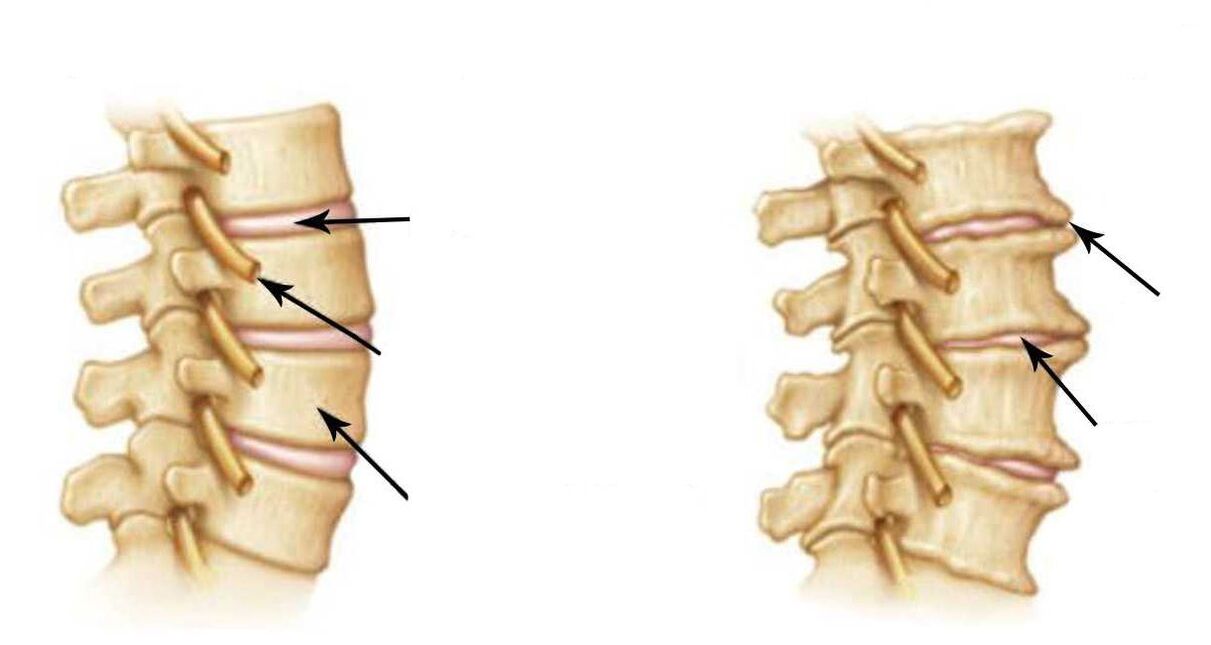
- Reduced disc height;
- Subchondral sclerosis;
- Marginal bone growth.
osteochondrosis


Causes of osteochondrosis
Signs and symptoms of osteochondrosis
- vertebrate/vertebrate
- Extravertebral/extravertebral: radicular symptoms and reflex symptoms

Diagnosis of osteochondrosis
Effective treatment of osteochondrosis
- consult. The doctor identifies the symptoms that are bothering the patient, clarifies the medical history, studies the patient's medical files, analyzes images and determines the nature of the disease.
- diagnosis. Perform a thorough examination and clinical examination of the patient: visual and myofascial diagnosis; palpation of tense muscles and painful vertebrae; neuroreflex testing and muscle testing.
- Treatment Plan. The doctor makes a diagnosis and selects a treatment plan based on the patient's current medical history, examination data, and clinical examination results. The doctor explains the nature of the disease and treatment principles to the patient in detail, and answers all the patients' questions.


















